Polycystic ovary syndrome (PCOS) is a common hormonal condition that affects how the ovaries function, particularly the menstrual cycle and ovulation. When asking yourself “What is PCOS?”, it’s important to understand that it is now viewed as a condition involving multiple body systems rather than a single organ. PCOS affects an estimated 1 in 10 women, though many remain undiagnosed for years.
Despite the name, polycystic ovaries are not always present; the term refers to the appearance of multiple immature follicles within the ovary, not true cysts, and some women meet diagnostic criteria without this finding on imaging.
At The Wellness Way, we take a personalized approach to helping women with PCOS who may be experiencing irregular or absent periods, lack of ovulation, insulin resistance, excess facial or body hair, infertility, weight gain, oily skin or acne, mood changes, abnormal uterine bleeding, or hormone imbalances.
While conventional care often focuses on symptom management with medications such as birth control or metformin, our focus is on identifying contributing factors and supporting hormone balance at the root level.
What causes PCOS
The cause of PCOS is unknown, and there is no single cause of PCOS that explains why the condition develops. Current evidence suggests that polycystic ovary syndrome arises from a combination of genetic, hormonal, and metabolic influences that interact over time rather than a single trigger.
- Insulin resistance: Reduced sensitivity to insulin can lead to high levels of circulating insulin. This may signal the ovaries to produce excess male hormones, contributing to hormonal imbalance and disrupting normal ovarian function.
- Androgen activity: Increased androgen production, including testosterone, can interfere with regular ovulation and contribute to physical changes such as acne, unwanted hair growth, and scalp hair thinning.
- Genetic susceptibility: PCOS often has a genetic component and may run in families, increasing the likelihood that women with PCOS have a family history of related metabolic or reproductive conditions.
- Inflammatory and metabolic influences: Low-grade inflammation and altered metabolic signalling may play a role in symptom development and can influence how hormones in your body interact over time.
- Body composition factors: Being overweight or having higher body fat accumulation can worsen insulin signalling and symptom severity, although weight alone does not explain why PCOS develops.
Overall, the cause of PCOS reflects overlapping biological processes rather than a single factor, which helps explain why the condition can present differently among females with PCOS.
Types of PCOS
You may see PCOS described in different “types.” These are clinical patterns based on hormone levels, ovulation, and ultrasound findings. They are not official diagnoses, but they can help explain why PCOS looks different from one person to another.
- Non-hyperandrogenic PCOS (Type D): This pattern involves problems with ovulation, which can lead to irregular or absent periods. An ultrasound may show polycystic ovaries, but androgen levels are within the normal range. women with this pattern often have cycle-related concerns without the more visible skin or hair changes linked to higher androgens.
- Ovulatory PCOS (Type C): In this pattern, androgen levels are elevated and polycystic ovaries may be seen on ultrasound, but ovulation still occurs. Periods may appear regular, which can delay recognition. Even with ongoing ovulation, higher androgen levels can still affect skin, hair, and metabolic health.
- Non-PCO PCOS (Type B): This pattern includes elevated androgen levels and ovulation problems, but the ovaries do not show a polycystic appearance on ultrasound. Cycle irregularity and androgen-related symptoms may still be present, even though imaging does not show typical ovarian changes.
- Full-spectrum PCOS (Type A): This pattern includes elevated androgens, irregular or absent ovulation, and polycystic ovaries on ultrasound. It reflects overlap across hormone, ovulation, and ovarian findings and is often the most easily recognized pattern clinically.
Symptoms of PCOS
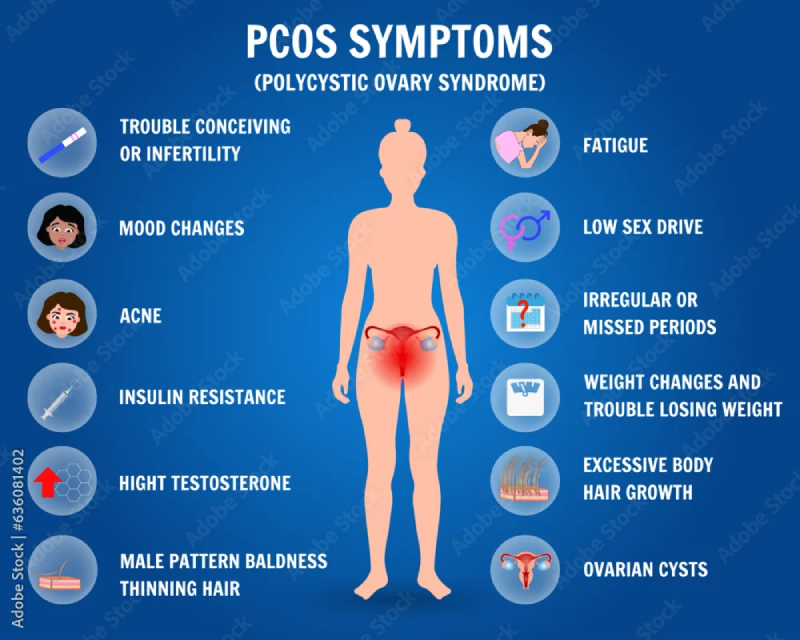
PCOS can look different from person to person. Some women notice several changes, while others have mild signs or none that stand out at first. Symptoms often relate to cycle timing, hormone levels, and metabolic patterns rather than a single issue.
- Menstrual cycle changes: Irregular or missed periods are common. Cycles may be unpredictable, occur infrequently, or stop for months at a time. Some women also notice heavier or prolonged bleeding when periods do occur. These changes usually reflect irregular ovulation.
- Skin and hair changes: Higher androgen levels can affect the skin and hair. This may include acne that continues beyond adolescence, oily skin, unwanted hair growth on the face or body, and thinning hair on the scalp. Some women also develop skin tags or darker patches of skin in body folds.
- Weight and metabolic patterns: Many women with PCOS find it easier to gain and harder to lose, especially around the abdomen. These patterns are often linked to insulin resistance rather than calorie intake alone. Energy dips, strong cravings, or feeling unwell when meals are delayed can also occur.
- Fertility and ovulation concerns: PCOS is a common cause of ovulatory infertility. When ovulation happens irregularly or not at all, it can be harder to conceive without support. This does not mean pregnancy isn’t possible, but timing can be less predictable.
- Emotional and mental health changes: Living with ongoing symptoms can affect mood and mental well-being. Anxiety, low mood, or depression are more common in women with PCOS and deserve attention as part of overall care.
- Mild or unnoticed symptoms: Some women have PCOS with few obvious symptoms. In these cases, the condition may only come to light during fertility evaluation, routine blood work, or when metabolic changes become more noticeable over time.
PCOS symptoms vary widely. Some changes are obvious, others develop slowly. Patterns over time often matter more than any single symptom.
Risk Considerations of PCOS
Several factors are associated with an increased likelihood of developing PCOS or experiencing more pronounced symptoms.
- Family and inherited patterns: A family history of menstrual disorders, type 2 diabetes, or related metabolic conditions is commonly observed, suggesting an inherited susceptibility rather than a single inherited trait.
- Metabolic strain: Impaired blood sugar regulation can place ongoing stress on the body and is often linked with broader metabolic changes that influence reproductive function.
- Body weight and fat distribution: Being overweight, carrying excess fat, or having increased abdominal weight around the belly is associated with more pronounced symptoms and higher cardiometabolic risk.
- Cycle regulation changes: Disruption in the signals that coordinate a normal menstrual cycle can contribute to irregular periods, even when symptoms appear mild.
- Inflammatory and environmental influences: Chronic low-grade inflammation and exposure to environmental endocrine disruptors may contribute to symptom expression in susceptible individuals.
- Lifestyle and long-term health factors: Conditions such as obesity, altered cholesterol levels, high blood pressure, and metabolic syndrome are seen more frequently and may influence symptom severity and long-term outcomes.
Conditions seen more often with PCOS
Women with PCOS are more likely to experience certain related health conditions.
- Type 2 and gestational diabetes
- Metabolic syndrome, involving blood sugar, blood pressure, and cholesterol changes
- Mental health concerns, including depression and anxiety
Hormonal and Reproductive Effects of PCOS
PCOS influences how hormones in your body interact, including estrogen, progesterone, and insulin-related pathways. When signaling is disrupted, the ovaries may not follow the usual pattern of egg development and release.
This can affect the lining of the uterus, particularly when cycles are infrequent. Over time, prolonged exposure to unopposed estrogen may increase the risk of endometrial cancer, which is why cycle regulation is clinically important.
- PCOS and hormones: PCOS alters hormonal balance in a way that affects both reproductive and metabolic systems. These changes help explain why symptoms may extend beyond menstrual irregularities.
- PCOS and fertility: Irregular or absent ovulation is a common reason PCOS affects fertility. Some women conceive naturally, while others need support to regulate ovulation. PCOS does not mean pregnancy is impossible, but timing can be less predictable.
- PCOS and menopause: Symptoms of PCOS can change with age. Menstrual cycles eventually stop at menopause, but metabolic and cardiovascular considerations may remain. Ongoing health monitoring can still be important later in life.
PCOS Diagnosis
The PCOS Diagnostic Criteria
PCOS is diagnosed using the Rotterdam Criteria, which requires any two of the following three features to be present after other conditions are excluded.
- Irregular or absent ovulation (oligo- or anovulation): This may present as infrequent, irregular, or absent menstrual periods and reflects disrupted ovulation.
- Hyperandrogenism: This may be clinical, such as excess facial or body hair and acne, or biochemical, shown by elevated androgen levels on blood tests.
- Polycystic ovarian morphology (PCOM): Identified on pelvic ultrasound, this refers to enlarged ovaries with multiple small follicles and does not require the presence of ovarian cysts.
Different combinations of these features result in recognized PCOS subtypes, which help guide clinical assessment and management.
Together, these systems-based assessments help us understand why PCOS symptoms may be presenting the way they are.
Recommended PCOS Testing
Once diagnostic criteria are met, we focus on understanding the underlying physiological factors that may be contributing to your symptoms.
- Food immune responses: We consider whether immune reactions to foods may be contributing to inflammation and hormonal imbalance.
- Hormone regulation over time: We assess how key reproductive hormones are being produced and metabolized, rather than relying on a single snapshot in time.
- Stress and cortisol signalling: We evaluate stress-response patterns that may influence insulin regulation and ovarian function.
- Gut health and digestion: We assess digestive function and microbial balance, as these play an important role in hormone processing and clearance.
- Thyroid and metabolic signalling: We evaluate thyroid function and its potential influence on cycle regularity, energy levels, and metabolic health.
The Wellness Way’s Root-Cause Approach to PCOS
To evaluate these systems in more detail, we may recommend targeted laboratory testing based on your symptoms and clinical findings.
- Immuno food allergy test: Used to identify immune responses to foods that may contribute to inflammation and hormonal disruption.
- Female hormone panel: Assesses baseline levels of estrogen, progesterone, and androgens.
- DUTCH complete hormone panel: Provides insight into hormone production, metabolism, and daily cortisol patterns.
- Genova GI Effects with parasitology: Evaluates digestion, gut microbiome balance, inflammation, and parasitic activity.
- Thyroid with hormones panel: Assesses thyroid function alongside related hormones that may influence cycles, energy, and metabolic health.
PCOS Treatment, Management, and Long-Term Health Considerations
PCOS management focuses on symptom control, cycle regulation, and reducing long-term health risks. Care is individual and may change across life stages.
Management Approaches Commonly Used for PCOS
Treatment plans are customized based on symptoms, health priorities, and reproductive goals.
- Lifestyle-based support: Nutrition, movement, sleep quality, and stress management may support metabolic health and cycle regulation.
- Medical management: Medications may be used to regulate menstrual cycles, manage androgen-related symptoms, or support ovulation when pregnancy is a goal.
- Symptom-specific care: Treatment may focus on concerns such as irregular periods, acne, unwanted hair growth, or hair thinning.
- Ongoing review: Management plans are reassessed and adjusted as symptoms, life stage, or reproductive plans change.
Long-Term Health Considerations With PCOS
PCOS is a long-term condition, and monitoring over time helps reduce future health risks.
- Metabolic health: Increased risk of insulin resistance, type 2 diabetes, and metabolic syndrome.
- Cardiovascular health: Blood pressure and cholesterol levels may require periodic monitoring.
- Fertility and reproductive health: Fertility patterns and pregnancy-related risks can change over time and may benefit from early assessment.
- Mental health: Anxiety and depression occur more frequently and should be addressed as part of ongoing care.
- Health changes with age: While menstrual symptoms may shift after menopause, metabolic and cardiovascular considerations can persist.
A Personalized Approach to PCOS Care
PCOS management is most effective when care is tailored to the individual. A personalized approach may include:
- Personalized nutrition and supplementation: Dietary guidance and supplement recommendations based on individual health history, symptoms, and metabolic needs.
- Reducing inflammation and metabolic strain: Strategies aimed at improving blood sugar regulation and addressing low-grade inflammation that may contribute to symptom patterns.
- Hormone-supportive lifestyle care: Support for stress management, sleep quality, and appropriate physical activity to promote overall hormonal balance.
- Environmental and detoxification considerations: Reducing exposure to hormone-disrupting chemicals and supporting normal liver function where clinically appropriate.
With appropriate assessment and ongoing care, many women are able to improve symptom control, support cycle regularity, and better manage long-term health.
PCOS FAQs
Can you have PCOS without cystson your ovaries?
Yes. A PCOS diagnosis does not require cysts to be present. While some ovaries contain a sac-like pattern made up of fluid-filled sacs, diagnosis is based on clinical criteria rather than imaging alone.
What are the signs and symptoms of PCOS?
The signs and symptoms of PCOS vary, but common features include irregular menstrual periods, acne, excessive hair growth, and weight changes. These common signs may develop gradually and differ between individuals.
Can you have PCOS without noticeable symptoms?
Yes. Some women have symptoms of polycystic ovary syndrome that are mild or easy to overlook. In these cases, PCOS may only be identified through blood work or fertility evaluation.
Is PCOS geneticor hereditary?
PCOS often runs in families. While no single gene has been identified, inherited factors increase susceptibility. This helps explain why the condition affects around 1 in every 10 women.
What causes PCOS symptoms?
PCOS can cause symptoms when hormonal and metabolic signals are disrupted. These changes may affect how the ovaries release eggs, influence hair patterns, and alter cycle regularity.
Can PCOS cause hair changes?
Yes. PCOS can contribute to excess hair growth on areas such as the chin, as well as hair loss on the scalp. Patterns vary depending on individual sensitivity to hormone changes.
Can you get pregnant naturally with PCOS?
Yes. Many women become pregnant without medical intervention. However, cycle timing can be unpredictable, particularly for those trying to get pregnant.
How does PCOS affect pregnancy?
PCOS and pregnancy outcomes vary. Once an egg is fertilized by a sperm, monitoring may be recommended due to higher rates of certain metabolic complications.
Does PCOS increase the risk of miscarriage?
PCOS has been linked to pregnancy loss in some individuals, particularly when metabolic factors are present. Risk varies and is influenced by overall health.
Is there a cure for PCOS?
There is no cure for PCOS. Management focuses on symptom control, cycle regulation, and long-term health rather than elimination of the condition.
Can PCOS affect sleepor breathing?
Yes. Conditions such as sleep apnea occur more frequently in women with PCOS, especially when metabolic risk factors are present.
Is PCOS the same as PCO or POS?
No. PCO and POS are informal or outdated terms sometimes used to describe ovarian appearance. They are not equivalent to a clinical PCOS diagnosis.
What hormones are affected by PCOS?
PCOS affects several hormonal pathways, which can influence metabolism, hair growth patterns, and reproductive timing.
Choosing The Wellness Way Approach
Hopefully, we helped answer the question “What is PCOS?” and explain why symptoms don’t always follow a clear pattern. At The Wellness Way, we take a personalized approach to care by looking beyond surface symptoms and using appropriate testing to better understand what may be contributing to your health concerns. Contact us or schedule a consultation to discuss next steps that support your long-term well-being.

